Tuesday, 11 July 2017
Lungs
Lung
From Wikipedia, the free encyclopedia
(Redirected from Lungs)
For other uses, see Lung (disambiguation).
| Lung | |
|---|---|

Diagram of the human lungs with the respiratory tract visible, and different colours for each lobe
| |

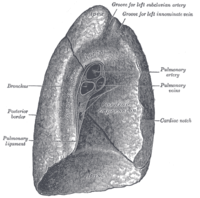
The human lungs flank the heart and great vessels in the chest cavity
| |
| Details | |
| System | Respiratory system |
| Identifiers | |
| Latin | pulmo |
| Greek | πνεύμων (pneumon) |
| MeSH | A04.411 |
| TA | A06.5.01.001 |
| FMA | 68877 |
| Anatomical terminology | |
The lungs are the primary organs of respiration in humans and many other animals including a few fish and some snails. In mammals and most othervertebrates, two lungs are located near the backbone on either side of theheart. Their function in the respiratory system is to extract oxygen from theatmosphere and transfer it into the bloodstream, and to release carbon dioxidefrom the bloodstream into the atmosphere, in a process of gas exchange.Respiration is driven by different muscular systems in different species. Mammals, reptiles and birds use their musculoskeletal systems to support and foster breathing. In early tetrapods, air was driven into the lungs by thepharyngeal muscles via buccal pumping, a mechanism still seen in amphibians. In humans, the primary muscle that drives breathing is the diaphragm. The lungs also provide airflow that makes vocal sounds including human speechpossible.
Humans have two lungs, a right lung and a left lung. They are situated within the thoracic cavity of the chest. The right lung is bigger than the left, which shares space in the chest with the heart. The lungs together weigh approximately 1.3 kilograms (2.9 lb), and the right is heavier. The lungs are part of the lower respiratory tract that begins at the trachea and branches into the bronchi and bronchioles and which receive air breathed in via theconducting zone. These divide until air reaches microscopic alveoli, where gas exchange takes place. Together, the lungs contain approximately 2,400 kilometres (1,500 mi) of airways and 300 to 500 million alveoli. Each lung is enclosed within a pleural sac which allows the inner and outer walls to slide over each other whilst breathing takes place, without much friction. This sac also divides each lung into sections called lobes. The right lung has three lobes and the left has two. The lobes are further divided intobronchopulmonary segments and lobules. The lungs have a unique blood supply, receiving deoxygenated blood sent from the heart for the purposes of receiving oxygen (the pulmonary circulation) and a separate supply of oxygenated blood (the bronchial circulation).
The tissue of the lungs can be affected by a number of diseases, includingpneumonia and lung cancer. Chronic diseases such as chronic obstructive pulmonary disease and emphysema can be related to smoking or exposure to harmful substances. Diseases such as bronchitis can also affect therespiratory tract. Medical terms related to the lung often begin with pulmo-, from the Latin pulmonarius (of the lungs) as in pulmonology, or with pneumo-(from Greek πνεύμων "lung") as in pneumonia.
In embryonic development, the lungs begin to develop as an outpouching of the foregut, a tube which goes on to form the upper part of the digestive system. When the lungs are formed the fetus is held in the fluid-filled amniotic sac and so they do not function to breathe. Blood is also diverted from the lungs through the ductus arteriosus. At birth however, air begins to pass through the lungs, and the diversionary duct closes, so that the lungs can begin to respire. The lungs only fully develop in early childhood.
Contents
[hide]Structure of the human lungs[edit]
"Meet the lungs" from the Khan academy
Gross anatomy[edit]
The lungs are located in thechest on either side of the heartin the rib cage. They are conical in shape with a narrow rounded apex at the top, and a broad concave base that rests on the convex surface of thediaphragm.[1] The apex of the lung extends into the root of the neck, reaching shortly above the level of the sternal end of the first rib. The lungs stretch from close to thebackbone in the rib cage to the front of the chest and downwards from the lower part of the trachea to the diaphragm.[1] The left lung shares space with the heart, and has an indentation in its border called the cardiac notch of the left lung to accommodate this.[2][3] The front and outer sides of the lung face the ribs, which make light indentations on their surfaces. The medial surfaces of the lungs face towards the centre of the chest, and lie against the heart, great vessels, and the carina where the trachea divides into the two main bronchi.[3] The cardiac impression is an indentation formed on the surfaces of the lungs where they rest against the heart.
Both lungs have a central recession called the hilum at the root of the lung, where the blood vessels and airways pass into the lungs.[1] There are also bronchopulmonary lymph nodes on the hilum.[3]
The lungs are surrounded by the pulmonary pleurae. The pleurae are two serous membranes; the outer parietal pleura lines the inner wall of the rib cage and the inner visceral pleura directly lines the surface of the lungs. Between the pleurae is a potential space called the pleural cavity containing a thin layer of lubricating pleural fluid. Each lung is divided into lobes by the invaginations of the pleura as fissures. The fissures are double folds of pleura that section the lungs and help in their expansion.[4]
The lobes of the lungs are further divided into bronchopulmonary segments based on the locations of bronchioles. Segments for the left and right lung are shown in the table.[5] The segmental anatomy is useful clinically for localising disease processes in the lungs.[5]
Right lung[edit]
| Right lung | Left lung |
|---|---|
Upper
| Upper
Lower
Lingula
|
The right lung has both more lobes and segments than the left. It is divided into three lobes, an upper, middle, and a lower, by two fissures, one oblique and one horizontal. The upper, horizontal fissure, separates the upper from the middle lobe. It begins in the lower oblique fissure near the posterior border of the lung, and, running horizontally forward, cuts the anterior border on a level with the sternal end of the fourth costal cartilage; on the mediastinal surface it may be traced backward to the hilum.[1]
The lower, oblique fissure, separates the lower from the middle and upper lobes, and is closely aligned with the oblique fissure in the left lung.[1][4]
The mediastinal surface of the right lung is indented by a number of nearby structures. The heart sits in an impression called the cardiac impression. Above the hilum of the lung is an arched groove for the azygos vein, and above this is a wide groove for thesuperior vena cava and right innominate vein; behind this, and close to the top of the lung is a groove for the innominate artery. There is a groove for the esophagus behind the hilum and the pulmonary ligament, and near the lower part of the esophageal groove is a deeper groove for the inferior vena cava before it enters the heart.[3]
Left lung[edit]
The left lung is divided into two lobes, an upper and a lower, by the oblique fissure, which extends from the costal to the mediastinal surface of the lung both above and below the hilum.[1] The left lung, unlike the right, does not have a middle lobe, though it does have a homologous feature, a projection of the upper lobe termed the “lingula”. Its name means “little tongue”. The lingula on the left serves as an anatomic parallel to the right middle lobe, with both areas being predisposed to similar infections and anatomic complications.[6][7] There are two bronchopulmonary segments of the lingula: superior and inferior.[1]
The mediastinal surface of the left lung has a large cardiac impression where the heart sits. This is deeper and larger than that on the right lung, at which level the heart projects to the left.[3]
On the same surface, immediately above the hilum, is a well-marked curved groove for the aortic arch, and a groove below it for the descending aorta. The left subclavian artery, a branch off the aortic arch, sits in a groove from the arch to near the apex of the lung. A shallower groove in front of the artery and near the edge of the lung, lodges the left innominate vein. The esophagus may sit in a wider shallow impression at the base of the lung.[3]

High-resolution CT scans of a normal thorax, taken in the axial,coronal and sagittal planes, respectively. Click here to scroll through the image stacks.
Respiratory system[edit]
Main article: Respiratory system

Respiratory system, which includes the upper and lower respiratory tract, of which the lungs are the major part.
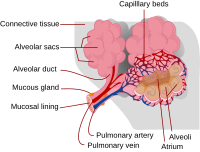
The lower respiratory tract is part of the respiratory system, and consists of thetrachea and the structures below this including the lungs.[8] The trachea receives air from the pharynx and travels down to a place where it splits (the carina) into a right and left bronchus. These supply air to the right and left lungs, splitting progressively into the secondary and tertiary bronchi for the lobes of the lungs, and into smaller and smaller bronchioles until they become the respiratory bronchioles. These in turn supply air through alveolar ducts into the alveoli, where the exchange of gases take place.[8] Oxygen breathed in, diffuses through the walls of the alveoli into the enveloping capillaries and into the circulation,[9] and carbon dioxide diffuses into the lungs to be breathed out.
Estimates of the total surface area of lungs vary from 50 to 75 square metres (540 to 810 sq ft);[8][10] roughly the same area as one side of a tennis court.[10][11]
The bronchi in the conducting zone are reinforced with hyaline cartilage in order to hold open the airways. The bronchioles have no cartilage and are surrounded instead by smooth muscle.[10] Air is warmed to 37 °C (99 °F), humidified and cleansed by the conducting zone; particles from the air being removed by the ciliaon the respiratory epithelium lining the passageways.[12]
Blood supply[edit]

3D rendering of a high resolution computed tomography of the thorax. The anterior thoracic wall, the airways and the pulmonary vessels anterior to the root of the lung have been digitally removed in order to visualize the different levels of the pulmonary circulation.
The lungs have a dual blood supply[8] provided by a bronchial and apulmonary circulation. The tissues of the airways, like the other tissues of the body, are perfused by normal systemic arterial blood. This blood constitutes the bronchial circulation which arrives via thebronchial arteries that leave the thoracic aorta. There are usually three arteries, two to the left lung and one to the right, and they branch alongside the bronchi and bronchioles.[8]
Most of the blood flowing through the lungs forms the pulmonary circulation. This arrives in the lungs via the pulmonary arteries from the right side of the heart.[8] This blood is then spread to the alveolar capillaries where the blood gases equilibrate with those in the alveolar air. The pulmonary capillary blood then drains into thepulmonary veins which return the blood to the left side of the heart, from where it is evenly spread to all parts of the body. The pulmonary circulation is in series with the systemic circulation, which means that the rate of blood flow, in litres per minute through the lungs, is equal to the rate of blood flow through the rest of the body.
The blood volume of the lungs, at any given moment, is about 450 millilitres on average, about 9 per cent of the total blood volume of the entire circulatory system. This quantity can easily fluctuate from between one-half and twice the normal volume.[13]
Nerve supply[edit]
The lungs are supplied by nerves of the autonomic nervous system. Input from the parasympathetic nervous system occurs via the vagus nerve. When stimulated by acetylcholine, this causes constriction of the smooth muscle lining the bronchus and bronchioli, and increases the secretions from glands.[14] The lungs also have a sympathetic tone from norepinephrineacting on the beta 2 receptors in the respiratory tract, which causes bronchodilation.[14]
The action of breathing takes place because of nerve signals sent by the respiratory centres in the brainstem, along thephrenic nerve to the diaphragm.[15]
Microanatomy[edit]
The lungs contain the respiratory tract and its lining, which terminate in alveoli, the lungtissue in between, and veins, arteries, nerves and lymphatic vessels.[3][16]
The lower respiratory tract begins with the trachea and bronchi. These structures are lined with columnar epithelial cells that possess cilia, small frond-like projections. Interspersed with the epithelial cells are goblet cells which produce mucus, and club cells with actions similar to macrophages. Surrounding these in the trachea and bronchi are cartilage rings, which help to maintain stability.[10] Bronchioles possess the same columnar epithelial lining, but are not surrounded by cartilage rings. Instead, they are encircled by a layer of smooth muscle.[10] The respiratory tract ends in lobules. These consist of a respiratory bronchiole, which branches into alveolar ducts and alveolar sacs, which in turn divide into alveoli.[3]
The epithelial cells throughout the respiratory tract secrete epithelial lining fluid (ELF), the composition of which is tightly regulated and determines how well mucociliary clearance works.[17][18]:Section 4 pages 7–8 (Page 4–7ff) which in turn is coated with a layer ofsurfactant.[8]
Alveoli consist of two types of alveolar cell and an alveolar macrophage. The two types of cell are known as type I and type II alveolar cells[8] (also known as pneumocytes).[3] Types I and II make up the walls and alveolar septa. Type I cells provide 95% of the surface area of each alveoli and are flat ("squamous"), and Type II cells generally cluster in the corners of the alveoli and have a cuboidal shape.[10] Despite this, cells occur in a roughly equal ratio of 1:1 or 6:4.[8][10]
Type I are squamous epithelial cells that make up the alveolar wall structure. They have extremely thin walls that enable an easy gas exchange.[8] These type I cells also make up the alveolar septa which separate each alveolus. The septa consist of an epithelial lining and associated basement membranes.[10] Type I cells are not able to divide, and consequently rely ondifferentiation from Type II cells.[10]
Type II are larger and they line the alveoli and produce and secrete epithelial lining fluid, and lung surfactant.[8] Type II cells are able to divide and differentiate to Type 1 cells.[10]
The alveolar macrophages have an important immunological role. They remove substances which deposit in the alveoli including loose red blood cells that have been forced out from blood vesels.[10]
The lung is surrounded by a serous membrane of visceral pleura, which has an underlying layer of loose connective tissueattached to the substance of the lung.[19]
Development[edit]
The development of the human lungs arise from the laryngotracheal groove and develop to maturity over several weeks in the foetus and for several months following birth.[20] The larynx, trachea, bronchi and lungs begin to form during the fourth week of embryogenesis[21] from the respiratory bud which appears ventrally to the caudal portion of the foregut.[22]
At the end of the fourth week the lung bud divides into two, the right and left primarybronchial buds.[23] During the fifth week the right bud branches into three secondary bronchial buds and the left branches into two secondary bronchial buds. These give rise to the lobes of the lungs, three on the right and two on the left. Over the following week, the secondary buds branch into tertiary buds, about ten on each side.[23] From the sixth week to the sixteenth week, the major elements of the lungs appear except the alveoli.[24] From week 16 to week 26, the bronchi enlarge and lung tissue becomes highly vascularised. Bronchioles and alveolar ducts also develop. During the period covering the 26th week until birth the important blood–air barrier is established. Specialised type I alveolar cells where gas exchange will take place, together with the type II alveolar cells that secrete pulmonary surfactant, appear. The surfactant reduces the surface tension at the air-alveolar surface which allows expansion of the terminal saccules. These saccules form at the end of the bronchioles and their appearance marks the point at which limited respiration would be possible.[25]
First breath[edit]
At birth, the baby's lungs are filled with fluid secreted by the lungs and are not inflated. After birth its central nervous systemreacts to the sudden change in temperature and environment. This triggers the first breath, within about 10 seconds after delivery.[26] Before birth, the lungs are filled with fetal lung fluid.[27] After the first breath, the fluid is quickly absorbed into the body or exhaled. The resistance in the lung's blood vessels decreases giving an increased surface area for gas exchange, and the lung begins to breathe spontaneously. This accompanies other changes which result in an increased amount of blood entering the lung tissues.[26]
At birth the lungs are very undeveloped with only a fraction of the alveoli present. The alveoli continue to form until the third year. Alveolar septa have a double capillary network instead of the single network of the developed lung. Only after the maturation of the capillary network can the lung enter a normal phase of growth. Following the early growth in numbers of alveoli there is another stage of the alveoli being enlarged.[28]
Function[edit]
Breathing[edit]
Main articles: Breathing and Rib cage § Function
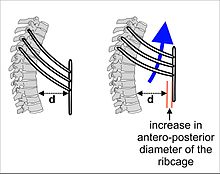
The lungs are not capable of expanding themselves, and will only do so when there is an increase in the volume of the thoracic cavity.[29]This is achieved by the muscles of respiration, through the contraction of the diaphragm, and the contraction of theintercostal muscles which pull the rib cage upwards as shown in the diagram on the right.[30] During breathing out, at rest, the muscles of inhalation relax, returning the chest and abdomen to a resting position determined by their anatomical elasticity.[30]At this point the lungs contain the functional residual capacity (FRC) of air, which, in the adult human, has a volume of about 2.5–3.0 litres.[30] This volume is needed to prevent the lungs from collapsing.
During heavy breathing as, for instance, during exercise, a large number ofaccessory muscles in the neck and abdomen are recruited.[30] Exhalation, instead of being passive, is now caused by the rib cage being actively pulled downwards at the front and sides by the abdominal muscles. This has the effect of decreasing the size of the rib cage, and of pushing the abdominal organs up against the diaphragm which bulges into the thorax. The lung volume of air at the end of exhalation is now less than than the resting FRC.[30] However, the lungs cannot be emptied completely and in an adult human there is always still at least one litre of residual air left in the lungs after maximum exhalation.[30]
Gas exchange[edit]
Main articles: Respiratory system and Gas exchange
The major function of the lungs is gas exchange between the blood gases and the alveolar air.[30] The alveolar andpulmonary capillary gases equilibrate across the blood–air barrier, a very thin diffusion membrane which is only, on average, about 2 μm thick,[31] consisting of the walls of the pulmonary alveoli, consisting of the alveolar epithelial cells, their basement membranes and the endothelial cells of the pulmonary capillaries.[30][31][32] This membrane is folded into about 300 million small air sacs called alveoli[31] (each between 75 and 300 µm in diameter) branching off from the bronchioles in the lungs, thus providing an extremely large surface area (estimates varying between 70 and 145 m2) for gas exchange to occur.[30][31]
The semi-stagnant volume of air (FRC)[note 1] always remains in the alveoli after a normal out-breath.[30] With each breath only about 350 ml (i.e. less than 15%) of this alveolar air is expelled into the ambient air (with about 150 ml remaining behind in the airways, as "dead space" ventilation, as it is the first air to re-enter the alveoli on inhalation).[30] This is immediately replaced with the same volume of fresh, but moistened, atmospheric air. It is therefore obvious that the 350 ml inhaled fresh air is highly diluted by the 3 litres of functional residual capacity air (i.e. the air that remains in the lungs after a normal exhalation), and that the composition of the alveolar air therefore changes very little under normal circumstances: the alveolar partial pressure of oxygen remains very close to 14 kPa ( 105 mmHg ), and that of carbon dioxide varies minimally around 5.3 kPa ( 40 mmHg ) throughout the respiratory cycle (of inhalation and exhalation).[30] Since the blood gasses in the alveolar capillaries equilibrate with those in the alveolar air, the arterial blood that is spread evenly throughout the body by the left ventricle, will have the same partial pressures of oxygen and carbon dioxide as persist in the alveoli.[30]
Control of breathing[edit]
The arterial partial pressures of oxygen and carbon dioxide in the arterial blood are homeostatically controlled. A rise in the arterial partial pressure of carbon dioxide, and, to a lesser extent, a fall in the arterial partial pressure of oxygen, will reflexly cause deeper and faster breathing till the blood gas tensions return to normal.[30] The converse happens when the carbon dioxide tension falls, or, again to a lesser extent, the oxygen tension rises: the rate and depth of breathing are reduced till blood gas normality is restored.[30]
It is only as a result of accurately maintaining the composition of the 3 litres alveolar air that, with each breath, some carbon dioxide is discharged into the atmosphere and some oxygen is taken up from the outside air. If more carbon dioxide than usual has been lost by a short period of hyperventilation, breathing will be slowed down or halted until the alveolar partial pressure of carbon dioxide has returned to 5.3 kPa ( 40 mmHg ).[30] The opposite occurs after breath-holding.
The partial pressures of oxygen and carbon dioxide in the arterial blood are measured by the "peripheral blood gas chemoreceptors" – the aortic and carotid bodies, and the "central blood gas chemoreceptors" of the medulla oblongata of the brainstem. The peripheral chemoreceptors are more sensitive to the arterial partial pressure of oxygen than they are to the arterial partial pressure of carbon dioxide.[30] The central chemoreceptor is particularly sensitive to the pH of thecerebrospinal fluid, which is directly influenced by the partial pressure of carbon dioxide in the arterial blood.[30][33]
Information from the blood gas chemoreceptors is relayed to a series of interconnected nuclei which comprise therespiratory centres in the medulla oblongata and the pons of the brainstem.[30] This information determines the average rate of ventilation of the alveoli of the lungs, to keep the partial pressures of oxygen and carbon dioxide in the arterial blood constant. The respiratory centre does so via motor neurons which activate the muscles of respiration (in particular thediaphragm).[15]
Exercise also increases the respiratory rate, partly in response to the movement of the limbs detected by proprioceptors in the muscles and joints, an increase in body temperature, the release of adrenaline (epinephrine) from the adrenal glands, and from motor impulses originating from the cerebral cortex.[34]
Subscribe to:
Comments (Atom)